About 1 in 3 with diabetes have an unknown heart risk: study
May 31, 2023 – If you have type 2 diabetes, you may already be at a higher risk for heart disease without knowing it. About a third of people with diabetes in a new study had higher levels of two things in their blood that are linked to heart disease.
These “biomarkers” in the blood can be detected before someone has symptoms of heart disease. So they could be used to screen people for higher risk earlier, at a time when prevention efforts or treatments may be more effective, researchers said.
“People with diabetes should be aware that they are at high cardiovascular risk and should work with their physician to develop a treatment plan that can prevent the future occurrence of cardiovascular events,” says senior study author Elizabeth Selvin, PhD, MPH, a professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health in Baltimore.
Historically, bad cholesterol has been blamed for a higher risk of cardiovascular disease in people with type 2 diabetes. This study suggests that something else is going on and that other types of treatments — besides those that lower cholesterol — should be considered.
“Our results suggest that hypertension treatment and interventions targeting microvascular or small vessel health may be particularly beneficial in people with diabetes,” Selvin said.
Heart under tension
Selvin, lead researcher Michael Fang, PhD, MHS, and their colleagues tested for two specific biomarkers. They found that 33% of people with type 2 diabetes had higher blood levels of one or the other, compared to only 16% of people without diabetes.
The study was published online today in the Journal of the American Heart Association.
One biomarker protein, called high-sensitivity cardiac troponin (hs-troponin), indicates damage to the heart. The other, called N-terminal pro-B-type natriuretic peptide (NT-proBNP), suggests that enough pressure is building in the heart to strain or stretch the heart wall.
Cardiovascular disease is linked to 40% of hospitalizations and 30% of deaths among people with type 2 diabetes, so it’s important to identify those at risk before symptoms begin. An estimated 27 million American adults have type 2 diabetes.
Large, diverse population
These two biomarkers have been studied before, but mostly in middle-aged or older white adults.
They are mainly measured in hospitals to test people with chest pain and/or shortness of breath. They are not generally used to identify heart disease, but emerging data such as this study suggest they may play a role in preventing or predicting risk, said Vijay Nambi, MD, a cardiologist at Baylor College of Medicine in Houston.
This current study tested stored blood samples from a more diverse, nationally representative group of 10,304 adults ages 20 and older. For example, of those with type 2 diabetes, 60% were non-Hispanic White, 15% non-Hispanic Black, 9% Mexican American, and 16% were of another race or ethnicity.
People in the study did not report heart disease when they participated in the National Health and Nutrition Examination Survey (NHANES) project between 1999 and 2004. By going back to stored blood samples from about 2 decades ago, Selvin and colleagues were able to predict deaths from heart disease. or other ailments. cause in the National Death Index until the end of 2019.
Main findings
A higher proportion of people with diabetes had higher levels of hs-troponin – 19%, versus 5% of those without diabetes. More muscle disease and frailty in people with diabetes could explain this difference, the researchers noted.
The researchers also found that the risk of heart disease was highest in people who had had diabetes for a longer period of time and whose blood sugar levels were less well controlled.
The other biomarker, NT-proBNP, was not significantly higher in the diabetes group. But those with diabetes and one or both biomarkers were more likely to die from diabetes or any cause. For example, the risk of cardiovascular death was 54% greater with elevated hs-troponin and 2.5 times more likely with elevated blood NT-proBNP levels in adults with type 2 diabetes. The risk of death from any cause was 77 % higher with hs-troponin and 78% higher with NT-proBNP in this population.
The higher risk persisted even after researchers controlled for other cardiovascular risk factors.
The risk of death was also higher in those ages 45 to 64, compared with those age 65 and older.
“These strategies need to be formally tested, but these biomarkers have consistently shown that they can identify individuals at higher risk. Therefore, one should generally seriously consider using these biomarkers on a routine basis,” Nambi said.
Screening for heart risk
Selvin and colleagues not only identified things that cause the higher risk, but also suggested what could be done about it.
“Our findings support the potential use of these cardiac biomarkers for routine risk monitoring, especially in high-risk populations, where we could use them to help tailor cardiovascular therapy,” Selvin said.
Using biomarker results to tailor management to an individual “would be even more powerful and effective,” agreed Nambi.
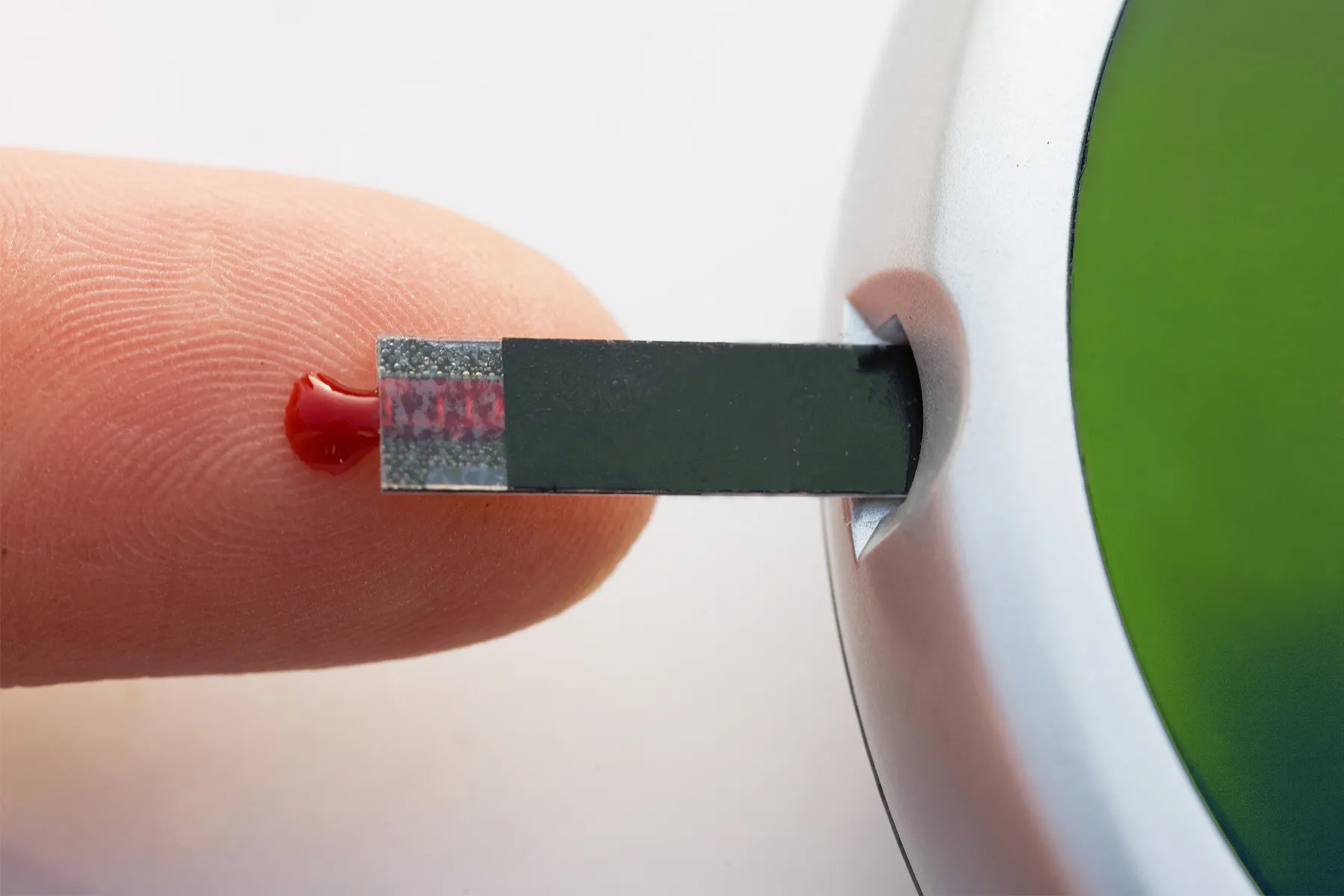
Taking a blood sample from people with type 2 diabetes to test for these two things could help prioritize who is being treated with a sodium-glucose cotransporter-2 (SLGT2) inhibitor, Selvin said. Drugs in the SLGT2 class include canagliflozin, dapagliflozin, and empagliflozin. The results could also guide treatment with a glucagon-like peptide-1 (GLP-1) receptor agonist. GLP-1 drugs such as semaglutide (Ozempic) and liraglutide (Victoza 3-Pak) have received a lot of attention recently for their weight loss potential.
More research is needed, Selvin said.
“We need to understand how best to use cardiac biomarkers in everyday practice to improve the lives of people with diabetes and other individuals at high risk of cardiovascular disease,” she said. “Intervention studies and clinical trials can be particularly helpful in informing best practices in this area.”
Stay connected with us on social media platform for instant update click here to join our Facebook
For the latest News and Updates, Follow Us on Google News
Read original article here












